Abstract
Background:
There is no standard cytoreductive regimen for patients with relapsed/refractory (R/R) acute myeloid leukemia (AML). Increasing evidence indicates the importance of epigenetic modification in the pathogenesis of myeloid neoplasms, and the epigenetic changes can be pharmacologically reversed by epigenetic modulating drugs (Halpern, Othus et al. 2017). Hypomethylating agents and histone deacetylase inhibitors showed chemo-sensitization when combined with conventional chemotherapeutics in patients with R/R AML (Halpern, Othus et al. 2017, Li, Wang et al. 2017). We conducted a phase 1/2 study of chidamide (a histone deacetylase inhibitor), decitabine (a hypomethylating agent), cytarabine, aclarubicin, and granulocyte colony-stimulating factor (CDCAG) for patients with R/R AML.
Methods:
This multicenter clinical trial evaluated the safety and efficacy of CDCAG regimen in patients with R/R AML (NCT02886559). Adults (age: 18-60) with R/R AML were eligible if they had not received treatment within 4 weeks prior to the enrollment. ECOG performance status ≤ 3 and expected survival time ˃ 3 months were required. All patients were treated with chidamide 30 mg on days 1, 4, 8, and 11; decitabine 20 mg/m2 on days 1-5; cytarabine 50 mg/m2 on days 1-7 if WBC ≥ 20×109/L, and on days 3-7 if WBC < 20×109/L; aclarubicin 10 mg/m2 on days 3-7; and granulocyte colony-stimulating factor, 300 ug/d until WBC > 20×109/L. Treatment cycles were repeated every 28 days. Patients could be treated for up to two cycles. Genomic DNA from patients at enrollment was examined for mutations by the target sequencing panel, which covered the coding sequences of 127 known genes relevant to the pathogenesis of AML (Annoroad Gene Technology Co., Ltd).
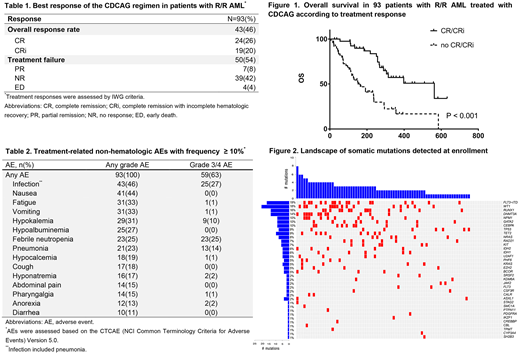
Results:
Ninety-three patients, median age 40 (range: 18-60) years, with primary refractory (n = 37), early relapsed disease (n = 38), or late relapsed disease (n = 18) were enrolled. Among the 56 patients with relapsed AML, 40 were experiencing their first relapse, 15 the second relapse, and 1 patient the third. They received a median of 5 (1-17) therapies cycles prior to the enrollment. Patients were enrolled on median 8.8 (1.3-63.8) months after initial diagnosis.
Overall, 24/93 (26%, 95% confidence interval [CI]: 16.9-34.7%) patients achieved a complete remission (CR) and 19/93 (20%, 95% CI: 12.2-28.4%) patients achieved a CR with incomplete blood count recovery (CRi), for an objective overall response rate of 46% (95% CI: 36.1-56.4%). Among the 43 CR/CRi patients, the 6-month disease-free survival (DFS) rate was 56% (95% CI: 41.0-70.7%), and the median DFS was 305 (95% CI: 258-NA) days. Patients achieving an CR/CRi had a significant improvement in median overall survival (OS) (259 vs 563 days; P < 0.001; hazard ratio [HR], 3.6) compared with nonresponders. The 6-month OS estimate was 52% (95% CI: 41.5-61.8%), and the median OS was 266 (95% CI: 235-398) days. Overall, we detected 184 mutations in 76 patients. Most commonly mutated genes were FLT3-ITD, CEBPA, WT1, RUNX1, and DNMT3A. Within patients with mutation, the CR/CRi rate was 55.6% in patients with epigenetic modifier gene mutations, and only 36.7% in patients with other mutations. Serious adverse events (SAE) occurred in 12 (13%) patients, with 4 patients experienced early death (death within 28 days). Only 1 patient died during consolidation.
Conclusions:
The CDCAG regimen was well tolerated and effective in relapsed/refractory AML. Compared with patients with other mutations, patients with epigenetic modifier gene mutations might benefit from the CDCAG regimen.
Disclosures
Chidamide tables were provided by Chipscreen Biosciences Ltd and decitabine was provided by Shandong New Time Pharmaceutical Co., Ltd.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal